The prevalence of desk jobs has surged in recent years to become widespread, transforming the way we work and how we interact with our professional environment. While these stationary roles offer conveniences and opportunities, they also bring to light a pressing concern: the heightened risk of Deep Vein Thrombosis (DVT) due to a sedentary lifestyle and lack of muscle movement in the legs.
In this article, we’ll provide an in-depth exploration of the intricate relationship between desk jobs and the development of DVT. By unraveling the myths about vein disease and discussing common practices that can negatively impact your circulation, we hope to provide simple adjustments that can help those who work sitting down to improve their circulation. Prioritizing your well-being while working in environments that can hinder your circulation requires little effort, and won’t disrupt your workday. Let’s get the blood pumping!
Deciphering Deep Vein Thrombosis (DVT)
Before delving into the connection between desk jobs and DVT, it’s important to understand and identify the signs and symptoms of Deep Vein Thrombosis.
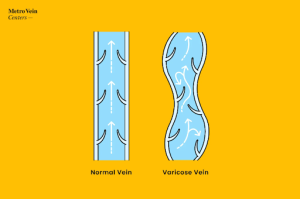
DVT is a serious vascular condition that most often occurs in those already suffering from moderate to severe vein disease, more specifically those who have varicose veins in their legs. People with varicose veins often experience blood clots, among other uncomfortable symptoms; DVTs occur when blood clots form within the deep veins in the legs. The concern with DVTs does not begin and end with the issue of circulation: if blood clots break free from the vein wall and travel to the lungs, a pulmonary embolism can occur which can be life-threatening. In addition, these clots (if not addressed) obstruct healthy blood circulation, leading to discomfort, pain, and the worsening of varicose veins.
DVTs are not always glaringly obvious, though; because they occur in the deep veins of the legs, it may not be noticeable like varicose veins that are closer to the surface of the skin and appear to be bulging, raised, and twisted. Because DVTs can seem somewhat asymptomatic (especially if someone has been dealing with varicose veins for some time) the more mild warning signs can mask the seriousness of such an issue. DVTs present with many of the same symptoms as varicose veins:
- Poor circulation
- Swelling
- Aching/heaviness in the legs
- Cramping legs
Something to note, however, is that DVTs have specific tells that can alert you to this serious condition. These differences are your body’s way of telling you that something is wrong that requires your immediate attention. The biggest sign? One-sided symptoms.
- Asymmetrical swelling: If only one leg is swelling or experiencing heat edema (skin that is warm to the touch on one leg only), this is a sign that you may have a blood clot in your deep veins.
- Aching/heaviness in one leg only: Because blood clots do not mirror each other, cramping from blood clots will very rarely occur in both legs at once. Take note if only one of your legs is aching!
- Skin and vein firmness: Your skin should be supple, not hard. If you notice that your skin or any visible varicose veins have hardened, seek medical attention immediately.
- Tenderness: If one of your legs is physically painful to touch, even gently (in the absence of cuts, wounds, bruises, or bug bites), this can be a sign of DVT.
- Discoloration/flushed skin: Darkening or reddening of the skin is another warning sign. This may be difficult to see on deeper complexions, but these symptoms rarely occur standing alone. If your skin is hot, swollen, or firm to the touch, or if your veins are visible when they usually aren’t, these can serve as warning signs if you cannot see the flush of blood so noticeably in your skin.
Decoding the Sedentary Connection
The immobile nature of desk jobs serves as a chief catalyst for the escalated risk of developing DVT. Prolonged periods of sitting, often accompanied by knees bent at right angles, lay the groundwork for sluggish blood flow. Reduced muscle activity, especially in the calf muscles (which are responsible for aiding blood return from the lower extremities to the lungs for re-oxygenation), compromises your veins’ ability to effectively pump blood back to the heart. Furthermore, the act of sitting induces vasoconstriction, adding an additional layer of restriction to natural, healthy circulation.
Sedentary behavior is not solely confined to the workplace; it extends to leisure time as well. After long hours at the office, many individuals tend to engage in sedentary activities such as lounging on the couch or using electronics at home in similar environments to their office. The cumulative effect of these behaviors increases the risk of DVT, making it imperative to address not only workplace practices but overall sedentary habits.
5 Tips for Improving Circulation
#1 Move: Set a timer to remind yourself to stand, stretch, and take a short walk every hour or so. The main focus is getting your calf muscles involved after a period of rest/stagnation. Do some calf raises while you grab coffee!
#2 Hydrate: Staying hydrated improves circulation as a whole, so keep a medium-to-large bottle or thermos nearby and try to finish it before you clock out.
#3 Exercise (out of the office): We know it can be difficult to motivate yourself to move after a long day of work, and especially difficult after a long workweek, but don’t worry! Low-impact exercises such as yoga, swimming, or walking are sufficient. Whatever your energy mobility level, there’s a movement or activity that will work with you.
#4 Compression Couture: Embracing compression stockings can be a discreet yet effective way to improve circulation. These specialized garments apply graduated pressure to the legs, discouraging blood pooling and clot formation. We recommend 20-30 mmHg, over-the-knee stockings for best results.
#5 Speak with a Vein Specialist: Vein disease is progressive, and worsens over time if left untreated. Moderate to severe vein disease can result in Deep Vein Thrombosis, which is largely avoidable with best practices and a proactive mindset. If you are experiencing pain, discomfort, or any common symptoms of vein disease, we recommend coming in for a free vein evaluation in any of our New York, New Jersey, Connecticut, Michigan, and Texas vein clinics. We offer minimally invasive vein treatments for varicose veins and spider veins and accept over 200 insurance plans (including Medicaid and Medicare).
If you suspect you’re suffering from vein disease, or DVT, our Metro Vein Center’s team of vein specialists can help.







