About one fifth of all diagnosed cases of breast cancer is a particularly aggressive form, known as triple-negative breast cancer (TNBC). TNBC lacks estrogen, progesterone, and ERBB2 receptors, making it difficult to treat effectively with few targeted therapies available. As such, the usual treatments of chemotherapy, surgery, radiation, and in some cases PARP inhibitors and immunotherapy are used. In an effort to further improve the current therapies, the FDA-approved medication mebendazole has been repurposed. This anthelmintic has the potential to be effective in treating cancer.
We investigated MBZ’s toxicity in humans and its efficacy in several different types of cancer, including breast cancer, glioblastoma multiforme, medulloblastoma, colon cancer, pancreatic, and thyroid cancer. Results of a human clinical trial concluded that MBZ has a good tolerance rate when given to adults with glioma. It was found that MBZ had a half-maximal inhibitory concentration (IC50) among four types of breast cancer cell lines that is comparable to other cancer types. Moreover, MBZ reduced the proliferation of TNBC cells, stimulated apoptosis, and arrested cells in the G2/M phase of the cell cycle. Additionally, it decreased the size of primary tumors and inhibited the formation of tumors in the lungs and liver. Furthermore, research uncovered a new action of MBZ, which is its ability to decrease ITGβ4 expression and eliminate cancer stem cell properties.
ITGβ4 has earlier been connected with enhancing “cancer stemness,” which could contribute to the productiveness of MBZ. Joining together our outcomes adds to forming proof that MBZ should be contemplated as a treatment to reduce the spread of tumors and ward off metastasis.
Introduction
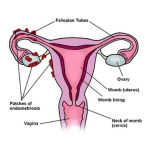
Breast cancer is the most widespread tumor among women, and results in more than 500,000 deaths per year among 2.0 million newly diagnosed cases. Pathologists utilize immunohistochemical (IHC) staining to identify hormone receptors such as the progesterone receptor (PR) and the estrogen receptor (ER), together with the human epidermal growth factor receptor 2 (HER2). For those with HR+/HER2−, HR+/HER2+, HR−/HER2+ diseases, there are targeted treatments available, however, triple-negative (TN) breast cancer, which lacks the usual HR and HER2, renders standard ER and HER2 therapies ineffective. This is particularly severe as TNBC is regularly linked to bone, brain, liver and lung metastases, making the development of new treatments essential for improving patient outcomes.
In 1971, the US Food and Drug Administration (FDA) permitted the use of Mebendazole (MBZ) to treat parasitic ailments. More recently, however, it has been evidenced that the drug also has preclinical usefulness in treating pancreatic, lung, thyroid, breast, meningioma, brain, melanoma, and colorectal cancers. The first reported manner of action for MBZ was the interference of tubulin. Tubulin happens to be targeted by multiple chemotherapy substances like paclitaxel, colchicine, and vincristine, surveying the preclusion of growth in cancer cells by MBZ.
MBZ has multiple anti-tumor features such as staunching of blood vessel growth, causing cell death by way of BCL-2 and caspase-3, halting cell division in the G2/M phase, and lessening of metastasis in previous tests on certain kinds of thyroid cancer. Although it was originally only tested on people with high-grade gliomas (in a phase 1 clinical trial, no less), it is now being investigated as a safe and workable remedy to breast cancer metastasis.
We hypothesized that MBZ might be an appropriate option for combating TNBC as there are limited treatments available and metastases are common. As is the case with many cancer types, we observed that MBZ induced apoptosis as well as stalled the cell cycle at G2/M. In addition to this, the expression of genes involved in angiogenesis and migration were inhibited. Moreover, we showed that MBZ could inhibit lung metastasis and eradicate liver metastases in tissue from breast cancer patients. Additionally, TNBC has particularly high levels of CSCs, which contribute to its viciousness.
The side effects of Mebendazole (MBZ) is shown to significantly reduce distant organ metastases in Triple Negative Breast Cancer (TNBC) models. This effect is believed to be due, at least in part, to the reducing integrin β4 (ITGβ4) expression levels that are observed with in vitro and in vivo cancer cell studies. This suppression of ITGβ4 curbs cancer stemness, suggesting the efficacy of MBZ to prevent metastatic spread.
Methods
Cell lines and cell culture
MDA-MB-231 (ATCC® HTB-26™) and 4T1 (ATCC® CRL-2539™) Mycoplasma-free breast cancer cell lines were obtained from American Type Culture Collection (ATCC) and cultured in DMEM (MDA-MB-231; Sigma-Aldrich) and RPMI-1640 (4T1; Sigma-Aldrich), both supplemented with 10% fetal bovine serum (FBS; Corning) and 1% penicillin/streptomycin (P/S; Invitrogen). SUM159 and 4T1-luciferase-tagged (4T1-Luc) cells from the Sukumar lab were cultured in Ham’s F12 medium with a mix of 5% FBS, 1% P/S, and 5% insulin/hydrocortisone (for SUM159) or 10% FBS and 1% P/S (for 4T1-Luc). All cells were grown in a humidified environment at 37°C with 5% CO2. MMTV-PyMT cells were derived from excised tumor tissue of a female triple-transgenic
Proliferation assays
The IC50 values for the MMTV-PyMT, MDA-MB-231, 4T1, and SUM159 cells were determined by adding 1000 cells in each well of a 96-well plate and treating them with 0.01-500 µM of mebendazole or less than 1% DMSO as the control. Following a 48-hour treatment period, 10% (v/v) concentration of PrestoBlue (Thermo Fisher) was added to every well, then left to incubate for 4 hours before measuring its fluorescence with the Cytation5 (BioTek Instruments). Values obtained from the nonlinear fit log vs. response model were then calculated as the IC50. Additionally, upon fixing cells in 70% ethanol, staining with DAPI and imaging through the Cytation 5 (BioTek Instruments) equipped with an Olympus–UPLFLN 4XPh phase objective and DMSO filter, the % cell survival was pinpointed.
A 4-by-3 layout was employed to register all of the regions of each well, and NIS Elements software (Nikon Instruments Inc.) was employed to set a limit on the DAPI advantageous locality of the picture, which is displayed as a % survival.
Colony formation assays
MDA-MB-231, 4T1, and SUM159 cells were placed in a 24-well dish (250 cells per chamber) and exposed to 0.01 – 1 µM of MBZ or DMSO, which served as the vehicle control, for 10 to 14 days (replenished every 3 days) or pre-treated with MBZ for 48 hours then placed in dishes without any further drug treatment. Subsequently, the cells were rinsed with 1 × phosphate-buffered-saline (PBS), fixed in 4% paraformaldehyde (PFA) in PBS for 15 minutes, then flushed with PBS again. A solution of 1% (w/v) crystal violet in a mixture of water and 20% methanol was added to every well and left to sit at room temperature for 10 minutes.
Wells were washed with distilled water and dried, after which they were imaged using the Cytation 5 (BioTek Instruments) with an Olympus-UPLFLN 4XPh phase objective. A 4 × 3 montage was taken to photograph the entire well. The number of colonies in each well was counted by hand.
Cell cycle analysis
MDA-MB-231 cells were exposed to 0.25, 0.5, 1, and 5 µM of MBZ and DMSO (as the vehicle control) for 48 h, then they were cleaned with PBS, fixed with 70% ethanol, and combined together and stained with RNase (100 µg/mL) and propidium iodide (50 µg/mL) in the dark at 4°C for an entire night. Flow cytometry using Beckman Coulter’s CytoFLEX flow cytometer was utilized to assess the cells in G1, S, and G2/M stages, and FlowJo software V10 performed the data analysis.
Western blotting
Cell homogenates were created by breaking down MDA-MB-231 and SUM159 cell lines or primary tumors generated by MDA-MB-231 cells with IGEPAL CA-630 buffer (150 mM NaCl, 1% IGEPAL CA-630, 50 mM Tris-HCl, pH 8.0, protease and phosphatase inhibitors) for ten minutes at cold temperature. The mixture was spun Down for 10 min at 13,000 g and 4 °C and the supernatant was removed. Proteins were then divided through a 10% sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) before being transmitted to a nitrocellulose membrane for thirty mins using the Trans-blot Turbo (Bio-Rad).
The membranes were soaked overnight in primary antibodies with a dilution of 1:1000 in 5% milk (w/v) in a 1 × Tris-buffered saline solution with 0.1% Tween-20 (TBS-T). Afterwards, the membranes were washed three times in TBS-T and incubated with HRP-conjugated secondary antibodies (Cell Signaling Technology). After three more washes, the chemiluminescence signal was captured by an AZURE C300 (Azure™ Biosystems) after incubating the membrane with ECL (Perkin Elmer). A listing of used antibodies can be found in Additional file 1: Table S1.
Transwell migration assays
In this study, the cells from two different sources, MDA-MB-231 and SUM159, were pre-treated with 0.5 or 1 μM of MBZ for 48 hours. The experiment was conducted on Costar Transwell’s cell culture inserts with 8-μM pore size PET membranes in a 24-well plate. The bottom chambers of the transwells were filled with 500 μL of the appropriate cell media, while the cells (20,000/well) were resuspended in 150 μL of 1% FBS medium and placed in the top well. After 24 hours, cells from the upper chamber were removed with a cotton swab, and those which migrated through the membrane were fixed with 100% ethanol and stained with 0.2% crystal violet dye.
Imaging of five spots on each pore was conducted with a Cytation 5 (BioTek Instruments) and a Olympus–UPLFLN 10XPh phase objective. To assess the MDA-MB-231 cells, a custom macro was run using ImageJ software with a view of conversion to 16-bit, changing the scale from pixel to µm, eliminating backgrounds with a rolling ball radius of 10 pixels and light background, and setting a boundary to show the crystal violet-positive regions of the wells.
The macro was changed to incorporate the color draw feature, the “hue” slider was utilized to emphasize the cell region, and the photos were handled at 8-bit to measure the % area for SUM159 cells.
Wound-healing assays
A 12-well plate was used to cultivate MDA-MB-231 and SUM159 cells, which reached almost full density within two days. A 200 μL pipette was used to produce equal length scratches. 0.25 μM, 0.35 μM, and 0.5 μM MBZ or DMSO (the control) was then added to the media. Pictures of the scraped region were taken at both 12 and 24 h using a Cytation 5 instrument connected to an Olympus-UPLFLN 4XPh phase objective. A combined image of the entire well was made by forming together the private images.
ImageJ software was utilized to quantify the healing rate and expanse of the wound. The macro we created changed them to 8-bit, set the scale to µm, included a Gaussian blur of radius 5 pixels, and utilized a threshold with the measure tool to just show the area created from the wound. The macro code measured the wound area in µm2 which was then joined by the full hours of the experiment (12 h or 24 h).
DNA extraction from mouse tissues
Mouse liver or lung tissues were incubated with Genomic DNA lysis buffer containing 1M Tris (at a pH of 8.0), 5M of NaCl, 0.5M EDTA, 10% Tween-20, 10% NP-40, and 40 μg proteinase K at 55°C for 3 hours with occasional vortexing. Subsequently, the proteinase K was inactivated with a brief heating step of two minutes at 95°C. The samples were then combined with a solution of phenol/chloroform/isoamyl alcohol (25:24:1) (Sigma), which was followed by 20 seconds of vortexing. Following this, centrifugation occurred for 10 minutes at 13,000 × g, resulting in the collection of the upper aqueous phase. Glycogen (20 μg), 0.1 volumes of 2.5 M NaCl, and 2 × volume of 100% EtOH were then added to the sample, where it was incubated for 20 minutes at − 20°C.
The samples were spun at 13,000 × g for 15 minutes to collect the DNA which was then washed with 70% ethanol. The spinning was then repeated for 5 minutes, afterward, the liquid was removed and the DNA pellets were left to dry. To make the pellets usable, they were suspended in DNase and RNase-free water before calculating the amount of human DNA contained in the mouse lung and liver by RT-PCR (by measuring the cycle threshold value of human hexokinase 2), then normalizing this to the DNA concentration (from 180 to 220 ng/µL) of the sample. To compare the results, each sample was normalized to the average value of the control group.
Reverse transcription and qPCR are methods of identifying and determining the amount of targeted nucleic acid molecules.
RNA was extracted with TRIzol (Invitrogen) followed by the conversion of the RNA into complementary DNA (cDNA) using Promega’s GoScript™ Reverse Transcriptase. Quantitative PCR (qPCR) was done on a CFX96 Real-Time PCR detection system (Bio-Rad) with a SYBR Green qPCR master mix (Bio-Rad). The expression of each target gene compared to the 18S rRNA control was measure with the Δ(ΔCt) strategy. This involved calculating ΔCt of the sample to be analyzed, which is equal to the Ct (target mRNA) minus the Ct (18S rRNA) followed by a comparison of ΔCt to the control group, expressed as Δ(ΔCt) which is ΔCt (treatment) minus ΔCt (control).
Please visit our website: https://www.fenbendazole.org/